Abstract
Introduction: Haploidentical hematopoietic stem cell transplantation (haplo HSCT) based on granulocyte colony-stimulating factor plus anti-thymocyte regimens ("Beijing Protocol") provides a salvage treatment for patients of acquired severe aplastic anemia (SAA) in China. However, graft-versus-host disease (GVHD) is a major impediment of haplo HSCT due to HLA disparity. Human umbilical cord blood (UCB) is characterized by lower numbers of mature or primed T-cells. Additionally, UCB has been reported to be a rich and rapidly accessible source of regulatory T cells (Tregs) and mesenchymal stromal cells (MSCs). These characteristics of UCB make it a potential prophylactic method for GVHD. Recently, haplo HSCT combined with umbilical cord blood (UCB) (haplo-cord HSCT) is performed in clinical trials to potentially reduce the risk of severe GVHD. Nevertheless, studies comparing GVHD in pediatric patients receiving haplo and haplo-cord HSCT for SAA are limited. Herein, we aim to investigate the impact of UCB co-infusion on GVHD in pediatric patients receiving haplo HSCT for SAA.
Methods: Data from 91 consecutive children with SAA treated with "Beijing Protocol"-based haploidentical transplantation with or without co-infusion of UCB between April 2015 and July 2021 in the Children's Hospital of Soochow University were retrospectively analyzed. The cohort included 35 patients in the haplo group and 56 patients in the haplo-cord group. All patients received uniform non-myeloablative conditioning, GVHD prophylaxis. We compared baseline characteristics and transplant outcomes between the haplo and haplo-cord recipients. Log-rank test and Cox proportional regression model were used for univariate and multivariate analysis, respectively. A significance level of 0.05 was used for all analyses.
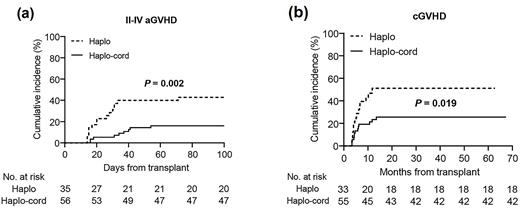
Results: No significant differences in the baseline information were observed between haplo and haplo-cord groups. All 91 patients achieved hematopoietic recovery from haploidentical donors, with a higher 30-day cumulative incidence of platelet engraftment observed with haplo group as compared to haplo-cord group (98.2% versus 97.1%, p = 0.028). Cox regression analysis revealed that the haplo or haplo-cord transplant type was not associated with the time to platelet engraftment, while a low CD34+ cell dose in haploidentical grafts was correlated with delayed platelet recovery (hazard ratio (HR), 2.495; 95% confidence interval (CI), 1.570-3.964; p < 0.001). The haplo-cord group showed a higher incidence of peri-engraftment syndrome compared to the haplo group (75.0% versus 48.6%, p = 0.029), and Cox regression analysis identified haplo-cord HSCT as the only significant factor associated with a higher incidence of peri-ES (HR, 1.767; 95% CI, 1.002-3.115; p = 0.049). Of note, the haplo-cord group showed a lower incidence of II-IV acute GVHD (aGVHD) than the haplo group (16.1% versus 42.9%, p = 0.002). Observed incidences of chronic GVHD (cGVHD) and moderate to severe cGVHD in the haplo-cord group were also lower than that in the haplo group (25.6% versus 51.3%, p = 0.019; 16.2% versus 41.3%, p = 0.016, respectively). Haplo-cord HSCT was identified as the only factor associated with a lower incidence of II-IV aGVHD (HR, 0.335; 95% CI, 0.143-0.784; p = 0.012) and cGVHD (HR, 0.429; 95% CI, 0.203-0.907; p = 0.027) in Cox regression analysis. No differences were observed between the two groups in CMV, EBV infection, overall survival, failure-free survival and GVHD, failure-free survival.
Conclusions: Our study provided compelling results of descriptive analysis suggesting that co-infusion of a third-party UCB unit with haplo HSCT might be associated with a lower risk of II-IV aGVHD and cGVHD. Although this co-infusion protocol may come with a higher risk of peri-ES, the survival outcomes may not be negatively affected. Despite the limited sample size, this study is the first real-world comparative study to investigate the impact of haplo-cord HSCT on GVHD in SAA children, which may stimulate further research of haplo-cord HSCT in pediatric patients with SAA and hematologic malignancies, as well as the potential association with GVHD.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.